Advertisment
Invasive melanoma procedure, harmful?
A special report published by the BMJ finds that thousands of melanoma patients around the world are undergoing an expensive and invasive procedure called sentinel node biopsy, despite a lack of clear evidence and concerns that it may do more harm than good.
Although not recommended for routine use in England, it has become the standard care for melanoma patients in several countries including the United States, where it was estimated to cost over $686m in 2012.
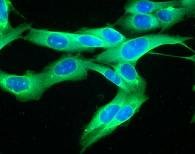
Melanoma is the fifth most common cancer in the UK, affecting one in 60 people. In the US it affects one in 50 people and, of the seven most common cancers, is the only one that is increasing. Sentinel node biopsy was developed in the US in the early 1990s to detect the early spread of cancer cells in patients with melanoma. It involves taking a small sample of the lymph node (gland) nearest to the melanoma for testing. If cancer cells are found, patients are advised to have surgery to remove some of the surrounding lymph nodes.
In 2006, a major trial (known as MSLT-I) published in the New England Journal of Medicine found that sentinel node biopsy did not improve overall survival after five years, yet the researchers claimed that disease-free survival was significantly higher in the biopsy group.
The results proved controversial, but further analyses of the data (expected around 2008 and 2011) that would have settled the question of effectiveness once and for all have not yet been published.
In 2007, the US National Cancer Institute, which funded the trial, accepted that it remained open to debate whether sentinel node biopsy should be standard care, but there has been no correction or clarification issued by the researchers or the journal. Nor has there been any public explanation about the delay in publishing the further analyses.
And when the BMJ contacted the lead researcher, he gave no timescale for when publication of the results could be expected.
Meanwhile, large numbers of patients are being exposed to unnecessary and potentially harmful surgery. It is thought that as many as 96% of patients who have sentinel node biopsy will have unnecessary surgery, which carries a risk of complications such as lymphoedema (severe swelling of the limbs), cellulitis (deep skin infection) and scarring.
In England, guidance from the National Institute for Health and Clinical Excellence (NICE) states that sentinel node biopsy should be performed only in centres with expertise in the context of clinical trials. Yet data obtained by the BMJ show that at least 19 trusts across England carried out sentinel node biopsy procedures on melanoma patients between 2006 and 2011.
The figures also suggest that in 2010-11, over 1,100 sentinel node biopsies could have been conducted at an estimated cost to the NHS of £7.6m. Given only two trials of sentinel node biopsy in melanoma are ongoing, this is likely to account for only a fraction of these biopsies.
The report concludes: “The full and final results of MSLT-I would clarify whether sentinel node biopsy is beneficial, and what, if any, its role in melanoma should be. It is time for the funders of MSLT-1 and those responsible for overseeing research to demand prompt publication of the full and final results of MSLT-I.”
Commenting on the report, BMJ Editor Dr Fiona Godlee, says the evidence that much research goes unreported is overwhelming, putting patients at risk and wasting healthcare resources. She calls on both industry and academia to clean up their act, and invites BMJ readers to sign up to www.alltrials.net – a campaign launched this week to ensure that all trials are registered and their results published.





