Understanding anticholinergic burden and its implications

29th EAHP Congress highlights
Anticholinergic burden (AB) or anticholinergic load (AL) refers to the cumulative effect of taking multiple medications with anticholinergic actions, which can lead to adverse effects, particularly in older adults, including cognitive impairment, falls, constipation and urinary retention. Two recent studies1,2 explored the problems associated with anticholinergic burden and the impact of pharmaceutical interventions.
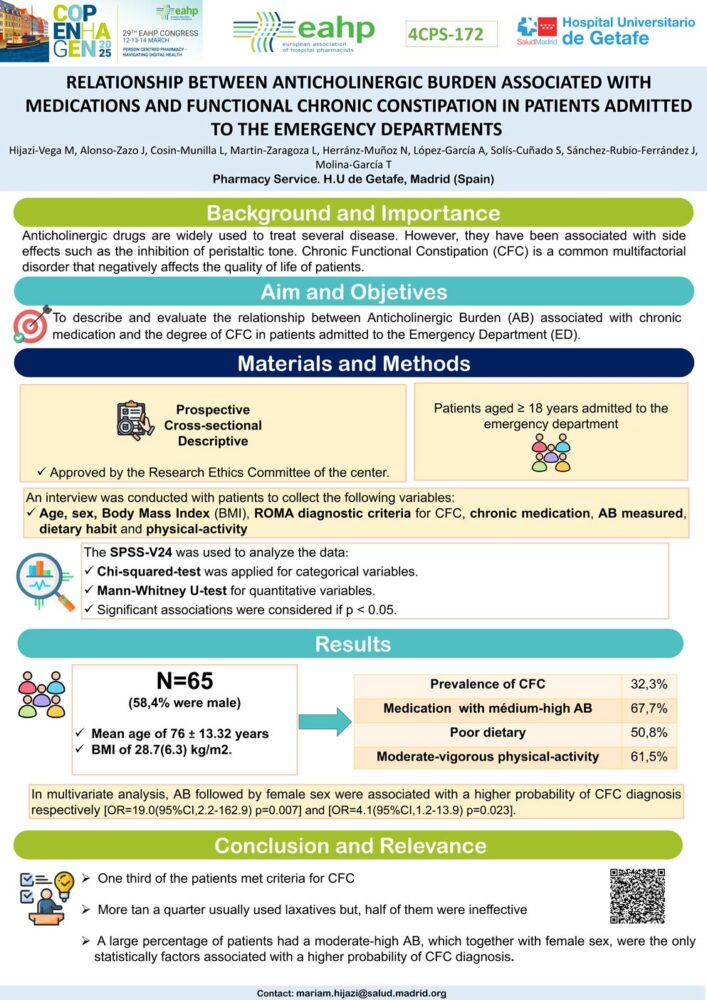
Mariam Hijazi and colleagues (University Hospital Getafe, Madrid, Spain) investigated the relationship between anticholinergic burden (AB) and the degree of chronic functional constipation (CFC) in patients admitted to the emergency department with at least one chronic medication. They reported that one-third of the 65 patients included in the study met the criteria for CFC. The mean age of participants was 76 years and a large proportion (67.7%) had medication with a medium-high AB. Multivariate analysis revealed that AB was significantly associated with a higher probability of CFC diagnosis [OR=19.0 (95% CI,2.2–162.9) p=0.007], along with female sex [OR=4.1(95% CI,1.2–13.9) p=0.023]. Although more than a quarter of participants usually used laxatives, half of them still met the criteria for constipation, suggesting that laxatives may be ineffective in the presence of significant anticholinergic burden.
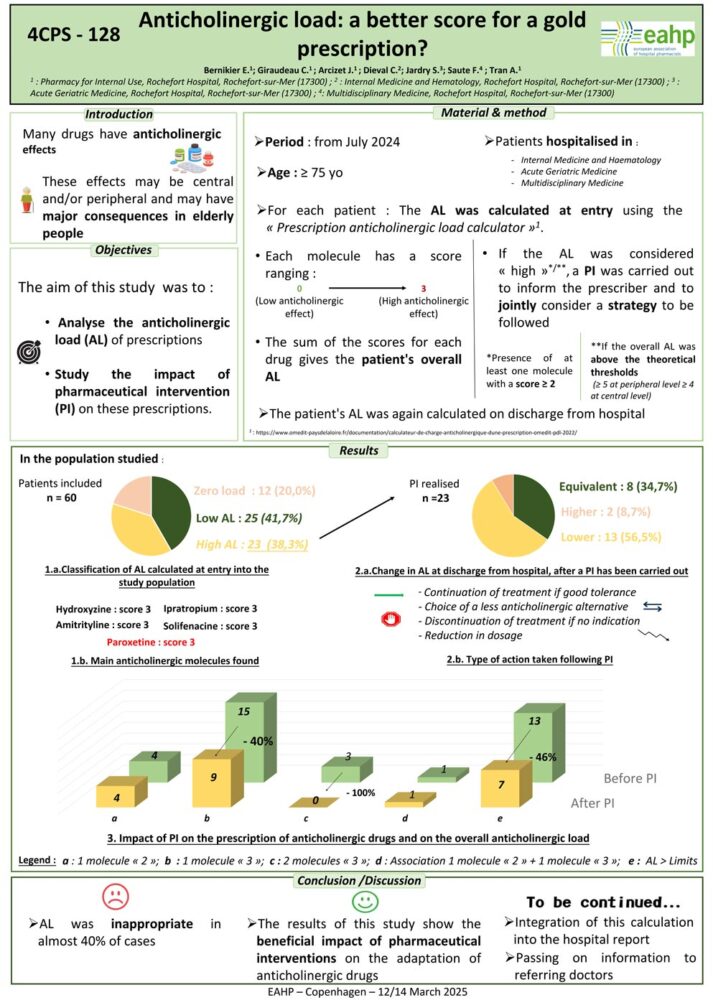
Bernikier and colleagues (Rochefort Hospital, France) focused on analysing the anticholinergic load (AL) of prescriptions in hospitalised patients aged 75 and older and the impact of pharmaceutical interventions (PI). AL was calculated at admission using a scoring system where each molecule received a score from 0 to 3 based on its anticholinergic effects. A prescription was considered to have a “high” AL if it contained at least one drug with a score ≥ 2 and/or if the overall AL exceeded predefined thresholds.
The study found that almost 40% (23 out of 60) of patients had a high AL at admission requiring a PI. Following PIs, which often involved switching to drugs with lower scores or discontinuing unnecessary treatments, a reduction in the discharge AL score was observed in 56% of patients. There was also a notable decrease in the number of patients taking drugs with the highest anticholinergic score (3) and a reduction in the number of patients exceeding the theoretical AL thresholds. The authors concluded that the calculation for AL should be integrated into hospital reports and the information be passed to referring doctors.
These studies underline the role of pharmacists in identifying and managing anticholinergic burden in elderly patients. In the hospital setting, proactive pharmaceutical interventions can significantly reduce anticholinergic load at discharge, potentially improving patient outcomes. This can involve suggesting dose adjustments, medication switches, or discontinuation of non-essential anticholinergic medications.
References
1. Hijaz Vega M, Alonso-Zazo J, Cosin-Munilla L et al relationship between anticholinergic burden associated with medications and functional chronic constipation in patients admitted to emergency departments. (Poster) EAHP Congress 2025
2. Bernikier E, Giraudeau C, Arcizet J et al. Anticholinergic load: a better score for a gold prescription? (Poster) EAHP Congress 2025