Advertisment
ILTS 2014: State of the art lecture: Transplantation or medical care for acute liver failure
Report from the Joint International Congress of ILTS, ELITA and LICAGE 2014. Roger Williams, Institute of Hepatology/Foundation for Liver Research, London, UK. Medical care after acute liver failure has improved greatly in recent years; meanwhile selecting candidates for liver transplantation after acute liver failure remains a considerable challenge due to the poor prognostic value of the current selection criteria. In the first of two State of the Art lectures at this year’s joint ILTS, ELITA and LICAGE congress, Professor Roger Williams, Director of the Institute of Hepatology and Foundation for Liver Research, discussed the role of liver transplantation and approaches to improving patient selection criteria, pointing out that in some indications, the added benefit of transplantation over medical care can be justifiably questioned.
Although the last 20 years have seen a dramatic improvement in survival rates, data from the European Liver Transplant Registry shows that overall survival after transplantation for acute liver failure remains approximately 10% lower than after non-acute liver transplantation [1]. However, after an initial steep drop due to early complications, the survival curve tends to level out within the first year thanks to younger patients and lack of recurrence of eg hepatitis C or hepatocellular carcinoma. At five and ten years post-transplant, patient and graft survival rates are not dramatically different from those after non-acute liver transplantation (patient survival 75% at five years, 72% at 10 years; graft survival 68% at five years; 63% at 10 years after liver transplantation for acute liver failure). Risk factors for mortality in the first year post-transplant include male gender, recipient age over 50, donor age over 60, and incompatible or reduced-size graft [1].
Alongside improvements in transplantation, medical care for acute liver failure has improved in leaps and bounds, mainly in the form of better knowledge and understanding of the underlying pathophysiology and early referral and renal replacement therapy protocols. Recently published data from King’s College Hospital show an increase in overall survival rate amongst over 3,000 non-transplanted acute liver failure patients, from 17% in 1973-78 to 48% in 2004-08 (p<0.0001) and a decrease in the rate of intracranial hypertension from 76% in 1984-88 to 20% in 2004-08 (p<0.0001) [2]. A recent prospective study in the United States reported an overall survival rate of 73% amongst patients with acute liver failure due to paracetamol overdose, which rose to only 78% after transplantation [3]. Leading experts including Professor Williams feel that the time is ripe for a policy review in light of these findings.
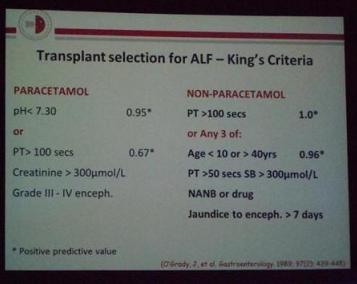
The King’s Criteria were published in 1989 and constitute a set of early prognostic indicators to select patients who are likely to benefit within the narrow time window in which transplantation is feasible (Table 1) [4]. However, a pooled meta-analysis of the prognostic value of the King’s Criteria showed that whilst the positive predictive value (specificity) was very high (95%) in paracetamol overdose cases and reasonable in non-paracetamol cases (81%), the negative predictive value (sensitivity) was unacceptably low in both aetiologies (58% and 68%, respectively) [5, 6]. Other models have been proposed for improving the prognostic scoring, such as utilising the MELD [7] or APACHE score [8] or measuring the M30 apoptosis marker [3]; however, the most promising approach in Professor Williams’ opinion is a prediction model developed at King’s College Hospital which is based on sequential analysis of all relevant criteria and which achieved an Area Under the Receiver Operating Characteristic Curve (AUROC) for prediction of 15-day survival of 0.95, compared with 0.78 for the standard King’s Criteria [9].
Professor Williams concluded by stressing that patient selection is key to improving outcomes and realising the potential benefit of liver transplantation in addition to state-of-the-art medical care for acute liver failure, but that in patients with a high probability of spontaneous recovery such as after paracetamol overdose, the added benefit of transplantation may be limited.
Table 1. King’s Criteria for transplant selection for acute liver failure [4].
References
1. Germani, G., et al., Liver transplantation for acute liver failure in Europe: outcomes over 20 years from the ELTR database. J Hepatol, 2012. 57(2): p. 288-96.
2. Bernal, W., et al., Lessons from look-back in acute liver failure? A single centre experience of 3300 patients. J Hepatol, 2013. 59(1): p. 74-80.
3. Larson, A.M., et al., Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology, 2005. 42(6): p. 1364-72.
4. O’Grady, J.G., et al., Early indicators of prognosis in fulminant hepatic failure. Gastroenterology, 1989. 97(2): p. 439-45.
5. McPhail, M.J., J.A. Wendon, and W. Bernal, Meta-analysis of performance of Kings’s College Hospital Criteria in prediction of outcome in non-paracetamol-induced acute liver failure. J Hepatol, 2010. 53(3): p. 492-9.
6. Craig, D.G., et al., Systematic review: prognostic tests of paracetamol-induced acute liver failure. Aliment Pharmacol Ther, 2010. 31(10): p. 1064-76.
7. Dhiman, R.K., et al., Early indicators of prognosis in fulminant hepatic failure: an assessment of the Model for End-Stage Liver Disease (MELD) and King’s College Hospital criteria. Liver Transpl, 2007. 13(6): p. 814-21.
8. Cholongitas, E.B., et al., King’s criteria, APACHE II, and SOFA scores in acute liver failure. Hepatology, 2006. 43(4): p. 881; author reply 882.
9. Al-Freah, M.A., et al., Comparison of scoring systems and outcome of patients admitted to a liver intensive care unit of a tertiary referral centre with severe variceal bleeding. Aliment Pharmacol Ther, 2014. 39(11): p. 1286-300.