Advertisment
Real-world data shows details beyond the clinical trials
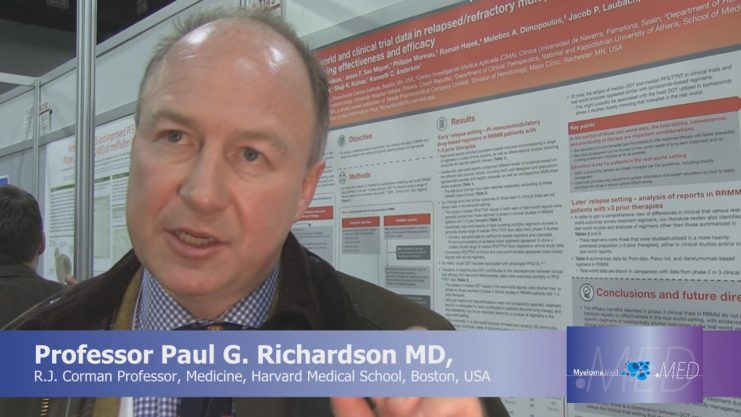
Professor Paul G. Richardson MD (R.J. Corman Professor, Medicine, Harvard Medical School, Boston, USA) and Dr Karthik Ramasamy (Oxford Oncology and Haematology Centre) discuss important learnings from real-world data, especially focussing on how the burden of side effects and ease of delivery can significantly impact on efficacy outside of clinical trials.
Articles by Thomas R Collins. Interviews by Esther Drain.
Clinicians treating multiple myeloma base their treatment decisions largely on data gleaned from Phase 3 clinical trials. But what happens after that, when the therapies are used not in a clinical trial, but in a clinic?
Researchers pursued this question in ‘real-world’ studies presented here at the Annual Meeting of the American Society of Hematology.
A study published earlier this year concluded that 40% of patients in an observational cohort would not be eligible to participate in randomised controlled trials under commonly used inclusion criteria, ruled out for low M-protein, high creatinine levels, low neutrophil counts, and low haemoglobin. Researchers also found that these patients had a lower 3-year survival rate on multiple myeloma therapies, when they were studied as part of a general population.
At ASH, researchers from a variety of centres in the U.S. and Europe presented findings1 comparing results for patients on clinical trials to real-world data gleaned from abstracts at myeloma trials over the last 3 years and a literature search covering the past 10 years. The real-world data was selected based on its relevance in being able to show comparisons with clinical trial data.
In some cases, researchers found, progression-free survival (PFS), or time to next treatment (TTNT) as a proxy for PFS, skewed lower in the real world than in clinical trials. For proteasome-inhibitor (PI) doublets or proteasome-based regimens, the PFS/TTNT range for bortezomib was 6.2 to 9.4 months in trials, compared to 5.7 to 11.9 in real-world studies. For carfilzomib, the range in trials was 14.9 to 22.2 months, compared to 3.2 to 9.4 months in the real-world studies.
Injectable PI-immunomodulatory triplet combinations had a PFS/TTNT of 18.3 to 29.6 months in the trials, but 9.4 to 12.7 months in the trials. For oral PI-IMiD triplet combinations, the real-world data dovetailed more closely with trial data — at 17.5 to 20.6 months in trials, versus 19.2 months in real-world data.
Researchers found that lower duration of therapy in trials versus the real world could be an important driver of these differences.
Among their observations, investigators said that “keeping patients on treatment through optimal toxicity management in the real-world setting is critical.”
In another study,2 researchers examining real-world data for patients receiving carfilzomib regimens found that those receiving carfilzomib-lenalidomide-dexamethasone (KRd) as second-line therapy had significantly improved time to next treatment, compared to those receiving bortezomib-lenalidomide-dexamethasone or bortezomib-cyclophosphamide-dexamethasone.
“Considering the real-world nature of these data,” said presenter Robert Rifkin, MD, medical oncologist at Rocky Mountain Cancer Centers, “the median TTNT observed with KRd appears to be consistent with the findings on progression-free survival for KRd in the phase 3 ASPIRE trial.”
References:
- Richardson P, Anderson K, Moreau P, et al. Real-World and Clinical Trial Data in Relapsed/Refractory Multiple Myeloma (RRMM): Evaluating Treatment Duration and Comparing Effectiveness and Efficacy. Abstract 3149. Presented December 10, 2017. Annual Meeting of the American Society of Hematology. Atlanta, Georgia.
- Rifkin R, Mezzi K, Panjabi S, et al. A Real-World Comparative Analysis of Carfilzomib and Other Systemic Multiple Myeloma Chemotherapies in the U.S. Community Oncology Setting. Abstract 3434. Presented December 10, 2017. Annual Meeting of the American Society of Hematology. Atlanta, Georgia.





