Advertisment
Video Interview and Report: Improving long-term outcomes in liver transplantation – the next paradigm shift?

As part of reports from the Joint International Congress of ILTS, ELITA and LICAGE 2014 with René Adam, Paul Brousse Hospital, Villejuif, France. Guiseppe Tisone, Tor Vergata University, Rome, Italy. Wolf Bechstein, Goethe University, Frankfurt, Germany.
With ever better immunosuppression regimens, outcomes in liver transplantation have improved beyond what anyone could have imagined when the first human liver transplantation took place in 1963 [1]. According to up-to-date registry data, 71% of patients and 64% of grafts are still alive five years post-transplantation [2] with current calcineurin inhibitor-based regimens. However, longer-terms outcomes remain suboptimal with reported 10-year survival rates of 62% for patients and only 54% for grafts in the most recent era [2]. Not only have increasing organ shortages and unmet demand for liver transplantation led to increasing use of extended-criteria organs from older donors and non-heart-beating donors, but liver transplant recipients are also reaching the transplant centres with more severe disease and as a consequence higher mortality risk [2, 3]. The challenge for clinicians and researchers is to optimise survival by optimising immunosuppression, and Astellas Pharma remains committed to supporting this quest. The first of two sponsored satellite symposia at this year’s joint ILTS, ELITA and LICAGE congress asked the question whether this can be achieved by optimising current immunosuppression regimens, and found that there is indeed room for improvement.
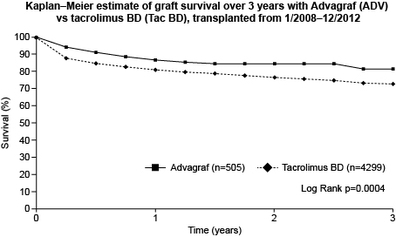
Professor René Adam presented data from over 4,000 liver transplantations recorded in the European Liver Transplant Registry (ELTR) which shows that administration of the once-daily prolonged-release formulation of tacrolimus (Advagraf®) within one month after transplantation significantly improves graft survival over three years compared with conventional twice-daily tacrolimus [4]. There was also an improvement in patient survival at three years, as shown in a poster and abstract by Professor Adam and co-workers presented at the congress [5]. The ELTR study was carried out as a retrospective observational analysis of all consecutive liver transplantations carried out in adult patients over a five-year period from January 2008 to December 2012, where the patient had received either Advagraf (n=548) or twice-daily tacrolimus (n=3,679) within the first month post-transplant. Risk factors influencing long-term graft and patient survival were analysed using multivariate and univariate Cox regression, survival was determined by Kaplan-Meier analysis, and Propensity Score Matching (PSM) was used to correct for baseline heterogeneity between the study groups.
The initial analysis showed a clear difference in graft and patient survival between patients receiving Advagraf and those treated with twice-daily tacrolimus. The overall graft and patient survival rates at three years post-transplant were 73% and 77%, respectively, with statistically significantly prolonged survival in the Advagraf group compared with the twice-daily tacrolimus group (graft survival: 82% versus 73%, p=0.0004; patient survival: 83% versus 76%, p=0.006; Figure 1) [5]. Treatment with twice-daily tacrolimus was identified as a significant risk factor of poor graft and patient survival (p=0.0004 and p=0.006, respectively), which was confirmed by multivariate analyses for graft survival (p=0.0175; relative risk [RR] 1.46; 95% confidence interval [CI] 1.07, 1.99).
Video interviews:
http://player.vimeo.com/video/99716419
http://player.vimeo.com/video/99721732
The fact that the difference in graft and patient survival between patients treated with Advagraf and twice-daily tacrolimus was evident already within the first three months of treatment led the team to hypothesise that there may be factors other than immunosuppression that influence the survival outcome. Further analyses were therefore carried out in a subset of patients who were followed for longer than one month post-transplantation. Univariate analysis identified a number of factors as significantly associated with poorer graft and patient survival at one and three years, including donor and recipient age, MELD score and renal function, as well as treatment with twice-daily tacrolimus. No difference was seen in graft or patient survival at one year post-transplant; however, at three years, graft survival was 87% in the Advagraf group compared with 81% in the twice-daily tacrolimus group (p=0.043). Patient survival was 87% and 83%, respectively; this difference did not reach statistical significance [4]. After further analyses using PSM to adjust for differences in donor age, incidence of hepatocellular carcinoma and MELD score between the two groups at baseline, there remained a survival difference in favour of Advagraf at two years (graft survival 91% versus 87% in the twice-daily tacrolimus group; patient survival 92% versus 88%) and three years (graft survival 88% versus 83%; patient survival 88% versus 85%) post-transplantation, although neither reached statistical significance due to the comparatively small sample size in the Advagraf (n=302) and twice-daily tacrolimus (n=604) groups in this analysis [4]. Professor Adam concluded that despite the usual limitations of retrospective data collection and lack of randomisation and blinding associated with this type of observational registry study, this data indicates a clear survival benefit with Advagraf over conventional twice-daily tacrolimus in a real-world setting that can be reasonably assumed to reflect state-of-the-art clinical practice. Professor Adam hypothesised that the two main factors contributing to the clinical benefit of Advagraf are likely to be improved adherence to therapy [6-9], and greater consistency of exposure [10, 11].
Video Interviews:
http://player.vimeo.com/video/99721735
http://player.vimeo.com/video/99721989
Professor Guiseppe Tisone has had long experience with using Advagraf after liver transplantation both in the de novo setting and following conversion from twice-daily tacrolimus. In his presentation at the satellite symposium, Professor Tisone shared data from his centre in Rome which comprises 542 liver transplantations carried out between July 1992 and December 2013, with a median follow-up time of 156 months and overall one- and five-year patient survival rates of 80% and 63%, respectively. A total of 170 patients have been treated with Advagraf at Professor Tisone’s centre; 86 patients received Advagraf de novo and 84 were converted from twice-daily tacrolimus. The first and most important message from Professor Tisone was that the plasma trough levels of tacrolimus achieved with Advagraf are very stable. Many clinicians are concerned that once-daily administration of tacrolimus will make correcting and stabilising trough levels more difficult, but in Professor Tisone’s experience this has not been the case. No episodes of acute rejection have been recorded at the Tor Vergata centre amongst liver transplant recipients receiving de novo Advagraf, and only eight patients (9%) developed renal impairment during treatment. Similar dosages and tacrolimus trough levels were recorded amongst patients receiving Advagraf as monotherapy and as part of a combination protocol with mycophenolate mofetil (MMF) and an mTOR inhibitor (mTORi).
Conversion from one immunosuppressive dosage form to another involves the risk of variability in exposure which in turn significantly increases the risk of graft failure [12]. However, published studies have shown that conversion from twice-daily tacrolimus to Advagraf reduces variability and provides more consistent and predictable exposure [10, 11]. Conversion to once-daily Advagraf has also been shown to improve treatment adherence [6]. The experience of conversion from twice-daily tacrolimus to Advagraf at Tor Vergata confirms these findings. To date, of 84 stable liver transplantation patients undergoing 1:1 conversion to Advagraf, only two had to go back to twice daily tacrolimus (one due to hypotension, vertigo and diarrhoea which developed at Day 43, and one due to recurrence of hepatocellular carcinoma which appeared on Day 215 post-conversion). No episodes of rejection were recorded, nor were there any deaths. More than three quarters of patients reported that they felt their quality of life had improved as a result of the conversion.
Video Interviews:
http://player.vimeo.com/video/99721733
http://player.vimeo.com/video/99721736
In the vast majority of cases (81%) no dose adjustment was required at 12 months post-conversion; a significant drop in mean tacrolimus levels was noted in the first three months after conversion, but by 12 months levels had returned to an acceptable, if slightly lower level. Professor Tisone concluded his presentation by encouraging clinicians to be brave and convert patients 1:1 since this is well-tolerated and helps to simplify immunosuppressive therapy and facilitate treatment adherence in the longer term.
Figure 1. Graft and patient survival at three years post-transplant [5].
Video Interview:
http://player.vimeo.com/video/99719929
References
1. Tolou-Ghamari, Z., Nephro and neurotoxicity of calcineurin inhibitors and mechanisms of rejections: A review on tacrolimus and cyclosporin in organ transplantation. J Nephropathol, 2012. 1(1): p. 23-30.
2. Adam, R., et al., Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol, 2012. 57(3): p. 675-88.
3. Eurotransplant International Foundation Annual Report, A. Rahmel, Editor. 2012: Leiden, The Netherlands.
4. European Liver Transplant Registry data on file. 2014.
5. Adam, R., et al., Prolonged-Release Tacrolimus (ADVAGRAF) Improves Survival Outcomes in De Novo Liver Transplantation: the European Liver Transplant Registry (ELTR). Liver Transpl, 2014. 20(6 (Suppl 1)): p. S188.
6. Beckebaum, S., et al., Efficacy, safety, and immunosuppressant adherence in stable liver transplant patients converted from a twice-daily tacrolimus-based regimen to once-daily tacrolimus extended-release formulation. Transpl Int, 2011. 24(7): p. 666-75.
7. Eberlin, M., G. Otto, and I. Kramer, Increased medication compliance of liver transplant patients switched from a twice-daily to a once-daily tacrolimus-based immunosuppressive regimen. Transplant Proc, 2013. 45(6): p. 2314-20.
8. Kuypers, D.R., et al., Improved adherence to tacrolimus once-daily formulation in renal recipients: a randomized controlled trial using electronic monitoring. Transplantation, 2013. 95(2): p. 333-40.
9. Valente, G., et al., Conversion from twice-daily to once-daily tacrolimus in stable liver transplant patients: effectiveness in a real-world setting. Transplant Proc, 2013. 45(3): p. 1273-5.
10. Florman, S., et al., Conversion of stable liver transplant recipients from a twice-daily Prograf-based regimen to a once-daily modified release tacrolimus-based regimen. Transplant Proc, 2005. 37(2): p. 1211-3.
11. Sanko-Resmer, J., et al., Renal function, efficacy and safety postconversion from twice- to once-daily tacrolimus in stable liver recipients: an open-label multicenter study. Transpl Int, 2012. 25(3): p. 283-93.
12. Lieber, S.R. and M.L. Volk, Non-adherence and graft failure in adult liver transplant recipients. Dig Dis Sci, 2013. 58(3): p. 824-34.