Expanding clinical pharmacy services – ESCP Day 2 Highlights
“Drug wastage jeopardises sustainability” was one of the driving concepts behind the ROAD (Re-dispensing unused oral anticancer drugs) project, according to Dr Charlotte Bekker (Radboud University Medical Centre). In The Netherlands the estimated cost of wasted drugs is 100 million Euros per annum. Re-dispensing of unused oral anticancer drugs was identified as being one way to reduce such wastage, although this not permitted in some countries, she acknowledged. Importantly, patients were happy to receive re-dispensed drugs, provided that the quality was assured by pharmacists. The initial study in four hospitals resulted in a 68% reduction in wastage and a projected saving of 20-30 million Euros per annum.
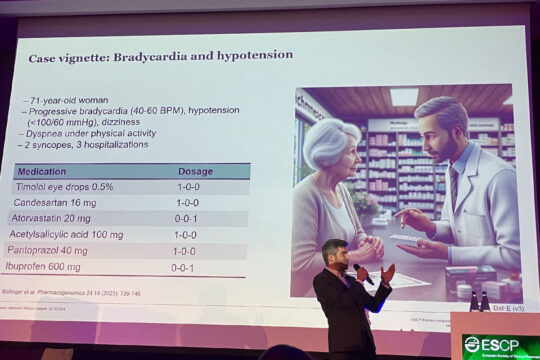
Pharmacogenomic testing
Professor Samuel Allemann and Dr. Markus Lampert described how pharmacogenomic testing might be implemented in clinical practice. Important prerequisites are the availability of point-of-care tests, and suitable insurance cover or reimbursement arrangements.
One case example clearly demonstrated the value of pharmacogenomic information: a 73-year-old woman had been prescribed timolol eye drops in addition to other regular medications. Since then she had developed bradycardia, hypotension, dizziness and breathlessness on exercise. She had suffered two episodes of syncope and had been admitted to hospital on three occasions. Timolol is absorbed into the systemic circulation and is rapidly metabolised by CYP 2D6. In this case pharmacogenomic testing revealed that she had loss of function variant of the enzyme and was unable to metabolise timolol. Her prescription was therefore changed to latanoprost eye drops.
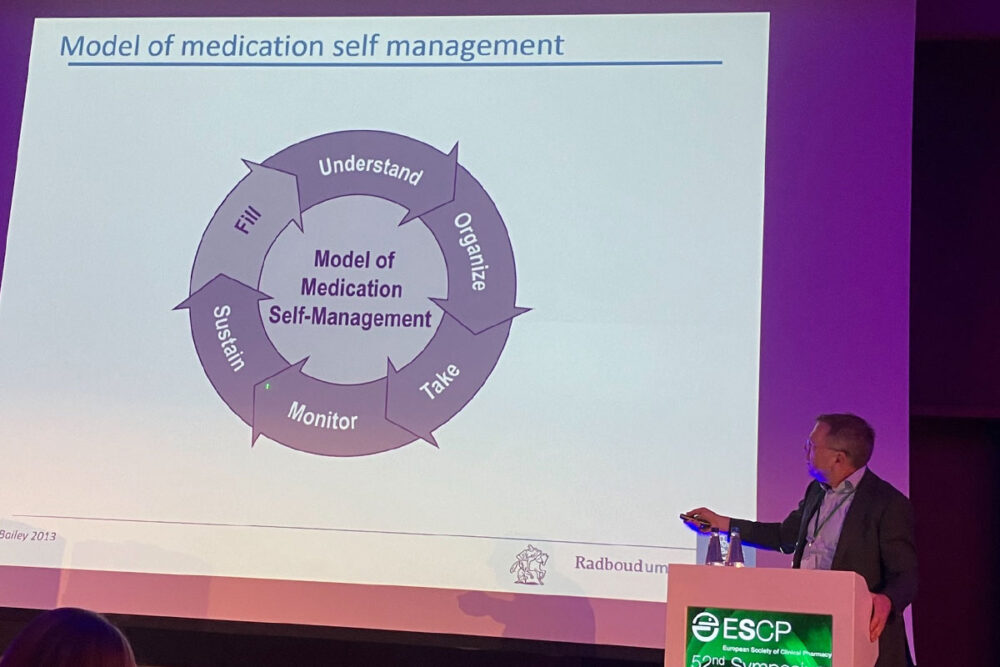
Rethinking clinical pharmacy services
“Clinical pharmacy services should have a sextuple aim”, Professor Bart van den Bemt told the audience. This should embrace not only effective and economical use of medicines but also wider aims of population health, healthcare providers’ health, environmental sustainability and equity. One of the keys to this would be to support self-management by patients. This would require significant efforts by pharmacist to use their skills and the available technology to inform and activate patients. For example, the answers to recurring questions can be built into websites and videos for patients. In one centre and avatar has been designed so that patients can put their questions directly to her. This helps people with poor health literacy who may not be able to formulate the ‘right’ question. ‘Activation’ means getting patients involved in contributing to their care for example by self-administration of medication in hospital or providing medication verification (reconciliation) at or before admission to hospital. “Digital services will really help us”, said Professor van den Bemt. His advice to pharmacists was to analyse critically how they spend their time and refocus on pharmaceutical care and the sextuple aim.





