What impact has the pulmonary embolism pathway had?
Evaluation of the new outpatient pulmonary embolism pathway showed that about 30% of patients could be managed safely and effectively via this route. Kieron Power, Principal Pharmacist for Thrombosis and Anticoagulation in Swansea Bay University Health Board, explains how this was achieved.
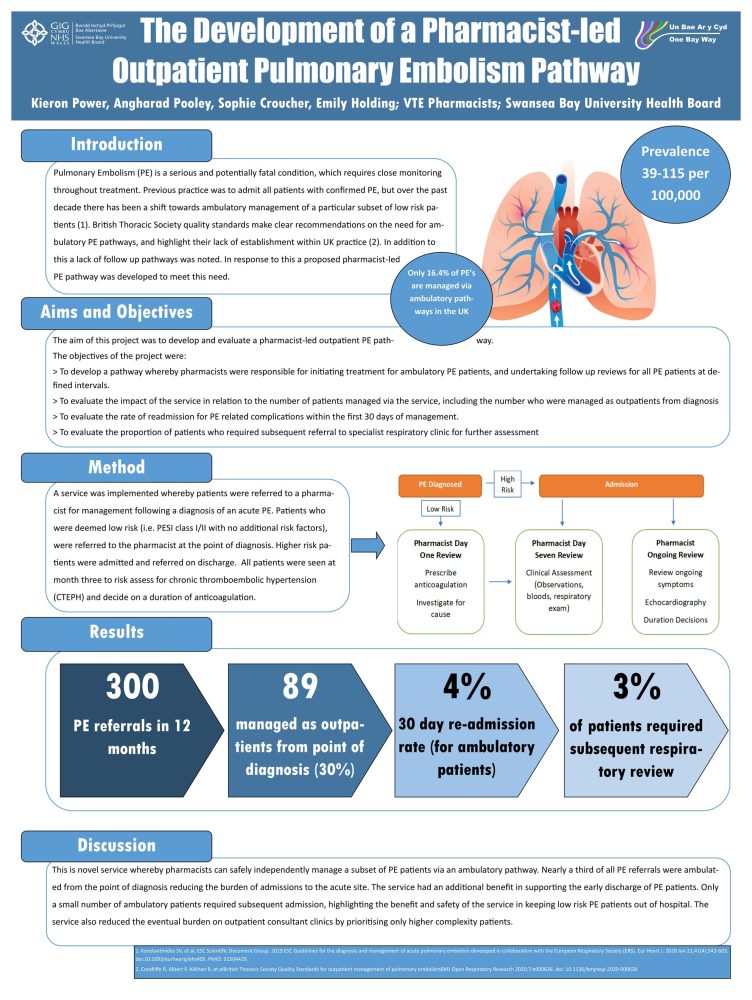
During the 12-month period September 2022 to the end of August of 2023 some 300 pulmonary embolism (PE) referrals were received. Of these, 89 were managed as ambulatory patients and the 30-day readmission rate was 4%. Furthermore, only 3% required referral to the respiratory team. These results showed that patients with low-risk PE could be safely managed as outpatients. “The idea is that these patients who are managed and recover well and don’t seem to have any complication – they were being kept out of those highly specialist services so that they could focus on the groups of patients who do need that specialist input”, said Mr Power. The numbers show that about 30% of patients were removed from the general PE pathway and managed safely and efficiently via the outpatient pathway.
The seven-day review is a critical aspect of the service. “These patients with the lower risk PEs – it’s still a very, very concerning event for them. …. There is quite a lot of anxiety for a patient with a PE so having that seven-day review is really useful from that perspective”, he emphasises. At the seven-day review patients undergo a full clinical assessment. As this is done in the Same-Day Emergency Care (SDEC) unit there is immediate access to other specialists if the patient’s clinical status is declining.
The pharmacists work as part of a multidisciplinary team (MDT) alongside senior GPs and consultant physicians. The out-patient PE pathway was developed in discussion with the other members of the MDT. “We had very productive discussions around pathways and such and it was for the better that we had those discussions because we were able to iron out some of the finer details”, recalls Mr Power.
One of the biggest challenges was tackling his own strongly-held view that further development of pharmacists’ advanced practice skills was required. Mr Power explains: “I was very keen for us as pharmacists to focus on what I feel our skills are – which is fundamentally in therapeutics. VTE, in general, is primarily a drug-managed condition – and especially in the groups of patients which we’re talking about – these lower-risk outpatients. But I feel that it’s a slightly more complex condition to understand [in terms of] what a good outcome looks like”.
A framework for practice has now been developed together with an extensive training programme. The advanced practice training ensured that “we actually add things on to our skills to make us better as prescribing clinicians within that area”, he says.
About Kieron Power
Kieron Power is Principal Pharmacist for Thrombosis and Anticoagulation in Swansea Bay University Health Board in South Wales. His role comprises three elements:
- Thrombosis and Anticoagulation Lead for the health board – a governance role that involves leading on policy and guidance within the Health Board and performance monitoring for hospital-acquired thrombosis rates, venous thromboembolism risk assessments and general anticoagulation prescribing factors.
- Running a weekly thrombosis and anticoagulation specialist clinic on behalf of the consultant haematologists.
- Leading and running the pharmacist-led acute VTE service and follow-up service that operate within the health board
Read and watch the full series on our website or on YouTube.
This episode of ‘In Discussion With’ is also on Spotify. Listen to the full podcast now.