Advertisment
Even with statins, high triglycerides may increase risk of second stroke
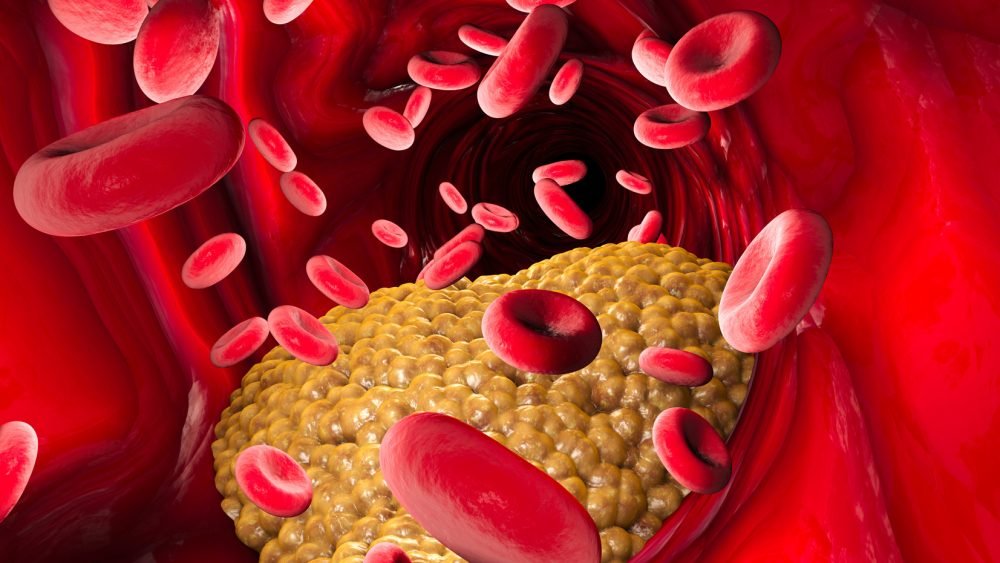
Stroke can have many causes. An atherothrombotic stroke is caused by a clot that forms from plaques that build up within blood vessels in the brain. A new study suggests that people who have this type of stroke who also have higher levels of triglycerides, a type of fat, in their blood may have a higher risk of having another stroke or other cardiovascular problems one year later, compared to people who had a stroke but have lower triglyceride levels. The research is published in the March 16, 2022, online issue of Neurology®, the medical journal of the American Academy of Neurology. The study found an association even when people were taking statin drugs meant to lower triglycerides and protect against heart attack and stroke.
Elevated triglyceride levels are thought to contribute to hardening of the arteries and increased risk of heart attack, heart disease and stroke.
“Our study suggests that for people who had atherothrombotic stroke, having elevated levels of triglycerides in their blood is a risk factor for having another stroke or other cardiovascular problems in the future, and we found that to be true even if the person is on statin therapy,” said study author Takao Hoshino, MD, of the Tokyo Women’s Medical University in Japan. “The good news is that statin medications are just one therapy for high triglycerides — diet and exercise can also be effective ways to reduce the levels in your blood at little or no cost.”
The study looked at 870 people who had a stroke or transient ischemic attack. Their average age was 70. Of those, 217, or 25%, had elevated triglyceride levels, defined as fasting triglycerides levels 150 milligrams per deciliter or higher.
Researchers followed up with the participants one year later to find out if there was an association between high triglyceride levels and having another stroke, acute coronary syndrome, which is any condition caused by a sudden reduction of blood flow to the heart, or death due to vascular causes.
After adjusting for factors like cholesterol level and statin use, researchers found that people who had high triglyceride levels had a 21% greater risk of death, stroke or heart condition one year, compared to 10% greater risk for those with lower levels.
When researchers looked specifically at people who had another stroke after an atherothrombotic stroke, they found that 14 out of 114 people with normal triglyceride levels, or 12%, had one during the study, compared to 33 out of 217 people, or 16%, of those with elevated levels.
For acute coronary syndrome, one out of 114 people, or 0.9%, with normal triglyceride levels developed the heart condition one year after an atherothrombotic stroke, compared to five out of 60, or 8%, of those with elevated levels.
Hoshino notes the study did not find an association between higher triglyceride levels and future cardiovascular problems in people who had a different type of stroke called cardioembolic stroke.
“More research is needed, but for people who have had an atherothrombotic stroke, triglyceride levels may emerge as a key target for preventing future strokes and other cardiovascular problems,” Hoshino said. “Statin therapy is still an effective treatment for people with high triglyceride levels, but our study highlights how important it is to look at all the tools a person can use to lower their triglycerides, including diet modifications, exercise and taking omega-3 fatty acids.”
The study does not prove that lowering high triglyceride levels will prevent people with atherothrombotic strokes from having cardiovascular problems later; it only shows an association.
A limitation of the study is that researchers considered only the participants’ fasting levels of triglycerides.
Journal Reference:
- Takao Hoshino, Kentaro Ishizuka, Sono Toi, Takafumi Mizuno, Ayako Nishimura, Sho Wako, Shuntaro Takahashi, Kazuo Kitagawa. Prognostic Role of Hypertriglyceridemia in Patients With Stroke of Atherothrombotic Origin. Neurology, 2022; 10.1212/WNL.0000000000200112 DOI: 10.1212/WNL.0000000000200112





